Deep Vein Thrombosis – Causes, Symptoms And Treatment
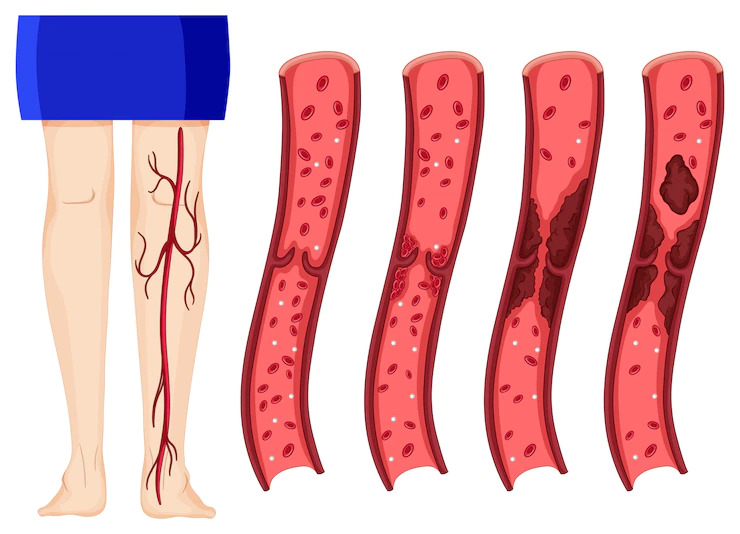
Deep vein thrombosis occurs when a blood clot (thrombus) develops in one or more of our body's deep veins, most often in the legs.
Author:Finn WildeReviewer:Michael RachalOct 04, 20222.8K Shares282.8K Views

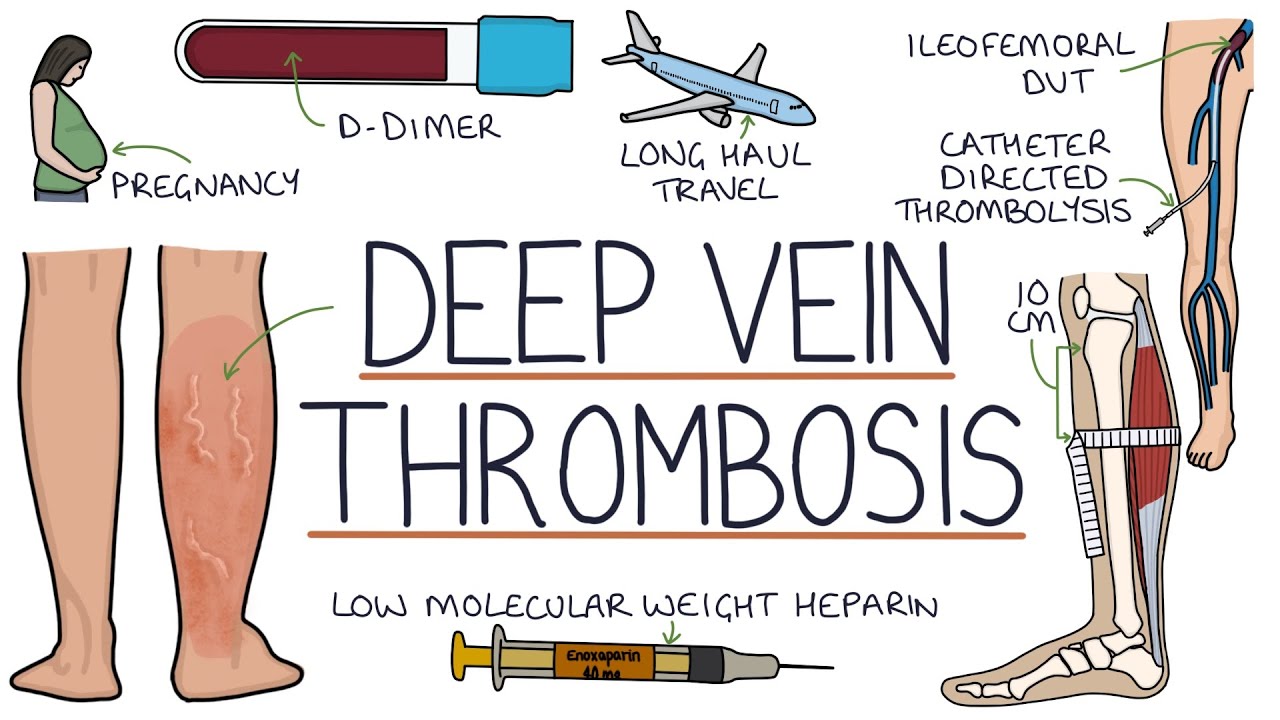
Deep vein thrombosisoccurs when a blood clot (thrombus) develops in one or more of our body's deep veins, most often in the legs. Deep vein thrombosis may cause limb discomfort or edema, but it can also develop without warning. Deep vein thrombosis may occur if you have specific medical issues that alter how your blood clots.
A blood clot in your legs may also occur if you do not move for an extended period, such as after surgery or an accident, after traveling a long distance, or when on bed rest. Deep vein thrombosis is dangerous because blood clots in your veins may break free, travelthrough your system, and get lodged in your lungs, obstructing blood flow (pulmonary embolism).
On the other hand, Pneumococcal embolism may develop in the absence of Deep vein thrombosis. When deep vein thrombosis and pulmonary embolism coexist, the condition is known as venous thromboembolism.
Understanding Deep Vein Thrombosis (DVT)
Causes Of Deep Vein Thrombosis (DVT)
A blood clot may be caused by anything that hinders your blood from flowing or clotting correctly. Deep Vein Thrombosis is caused mainly by damage to a vein caused by surgery or trauma and inflammation caused by infection or injury. Several risk factors lead to the development of deep vein thrombosis:
- Surgery, especially hip or leg surgery or stomach surgery
- A fractured bone or a traumatic injury
- A prolonged duration of bed rest or prolonged sitting (e.g., on an airplane or in a car)
- Hormones or birth control tablets used to treat menopausal symptoms
- Varicose veins
- Being over the age of 60 increases your chances of developing Deep Vein Thrombosis, which may happens at any age.
- Extended bed rest, such as during a hospital stay or paralysis. Blood clots may develop in the calves of your legs if you don't activate your calf muscles for an extended length of time.
- Pregnancy raises the pressure in your pelvic and leg veins. Women who have a genetic clotting condition are more vulnerable. The danger of blood clots during pregnancy might continue for up to six weeks after your baby is born.
- Obesity or being overweight. Obesity raises the pressure in the veins in your pelvis and legs.
- Smoking interferes with blood coagulation and circulation, increasing your risk of Deep Vein Thrombosis.
- Some types of cancer raise the levels of chemicals in your blood that cause it to clot. Some cancer treatments can increase the risk of blood clots.
- You are more likely to get Deep Vein Thrombosis and pulmonary embolism. Because persons with heart failure have impaired heart and lung function, even a minor pulmonary embolism causes more visible symptoms.
- Deep Vein Thrombosis risk is increased by bowel illnesses such as Crohn's disease or ulcerative colitis.
- An individual or family history of Deep Vein Thrombosis. If you or a family member has had one or both, you may be more likely to get Deep Vein Thrombosis.
- Some people inherit genetic risk factors or disorders, such as factor V Leiden, that make their blood clots more easily. An inherited disorder on its own might not cause blood clots unless combined with one or more other risk factors.
- There is no identified risk factor. A blood clot in a vein might form when there is no obvious risk factor.
Deep Vein Thrombosis Symptoms
The following are some of the most common deep vein thrombosis symptoms:
- Swelling on one side of your foot, ankle, or leg
- cramping discomfort in the afflicted leg, which commonly starts in the calf.
- acute, inexplicable foot and ankle pain
- a patch of skin that is warmer than the skin around it
- Depending on skin tone, the skin over the afflicted region may become pale, reddish, or blue.
People may not realize they have DVT until they have received emergency treatment for a pulmonary embolism (blood clot in the lung). A pulmonary embolism occurs when a DVT clot travels from the arm or leg to the lung. When an artery in the lung gets clogged, it is a life-threatening situation that needs immediate medical attention.
Deep Vein Thrombosis Treatment
Treatment options for Deep Vein Thrombosis include:
- Thinners of the blood Anticoagulants:often known as blood thinners, are the most widely used treatments for Deep Vein Thrombosis. These medications do not dissolve existing blood clots, but they may keep clots from becoming more extensive and lower your chance of acquiring new chunks. Blood thinners may be administered orally, intravenously, or subcutaneously. Heparin is commonly administered intravenously. Enoxaparin (Lovenox) and fondaparinux are the most widely used injectable blood thinners for Deep Vein Thrombosis (Arixtra). After a few days of using an injectable blood thinner, your doctor may decide to switch you to a tablet. Warfarin (Jantoven) and dabigatran are two examples of blood thinners that you may take (Pradaxa). Certain blood thinners do not need to be administered first through an IV or injection. These medications include rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). They may be begun as soon as a diagnosis is made. You may need to take blood-thinning medication for three months or longer. To avoid significant side effects, it is essential to take them precisely as directed. If you take warfarin, you will need frequent blood tests to determine how long it takes your blood to clot. Pregnant women should not use certain blood-thinning drugs.
- Clot dissolvers:These treatments, also known as thrombolytics, may be administered if you have a more dangerous kind of Deep Vein Thrombosis or if other medications aren't working. These medications are administered intravenously or through a tube (catheter) inserted directly into the clot. Clot busters may cause significant bleeding. Hence they are often reserved for people with severe blood clots.
- Filters:If you cannot use blood-thinning medications, a filter may be put into a central vein in your belly called the vena cava. A vena cava filter prevents blood clots from becoming lodged in your lungs.
- Stockings with compression:These particular knee socks lessen the likelihood of your blood pooling and clotting. Wear them on your legs from your feet to around the level of your knees to help reduce swelling caused by deep vein thrombosis. If feasible, you should wear these stockings for at least two years throughout the day.
Can Deep Vein Thrombosis Go Away On Its Own?
Deep vein thrombosis is most often seen in the lower leg. It usually goes undetected and disintegrates on its own. However, it may induce symptoms such as discomfort and edema. If someone has Deep vein thrombosis, they will need therapy to prevent significant consequences such as pulmonary embolism.
What Does A Thrombosis Feel Like?
Throbbing or cramping discomfort in one leg (sometimes both), often in the calf or thigh. Warm skin surrounding the sore region, swelling in one leg (occasionally both legs). Skin that is red or discolored around the painful spot.
How Can I Dissolve A Blood Clot In My Leg Naturally?
Consume fresh pineapple or a bromelain-containing dietary supplement. Consume more foods and beverages that may help dissolve blood clots, such as garlic, kiwi, kale, spinach, red wine, and grape juice. Drink plenty of water. Increase your physical activity.

Finn Wilde
Author
For Finn Wilde, the wilderness is more than just a destination - it’s a way of life. Over the past decade, he has led multiple expeditions in some of the world’s most remote regions, from the icy fjords of Greenland to the rugged trails of Patagonia.
Finn emphasizes sustainability in all of his adventures, helping participants connect with nature while promoting responsible exploration. His expeditions inspire individuals to explore the great outdoors while fostering a deep respect for the environment.

Michael Rachal
Reviewer
Michael Rachal believes that luxury lies in the details. With over 20 years of experience in the luxury travel industry, he has crafted hundreds of bespoke itineraries for clients seeking personalized, unforgettable experiences.
Whether guiding clients through private cultural tours or curating culinary journeys with world-renowned chefs, Michael ensures that each trip is tailored to perfection.
His ability to anticipate needs and exceed expectations has earned him a reputation as a leading expert in luxury travel.
Latest Articles
Popular Articles